Three separate smallpox escapes [1966, 1972, and 1978] occurred at two different accredited UK smallpox laboratories causing at least 80 cases and 3 deaths. In 2007, Foot and Mouth disease escaped from high security UK lab at Pirbright at a cost to the UK economy of 200 million pounds [$284 million US]. 3/31/2014, “Threatened pandemics and laboratory escapes: Self-fulfilling prophecies," Martin Furmanski, Bulletin of the Atomic Scientists
“Smallpox releases in Great Britain
Eradication of natural smallpox transmission made the prospect of reintroduction of the virus intolerable. This risk was clearly demonstrated in the United Kingdom, where from 1963-1978 only four cases of smallpox (with no deaths) occurred that were imported by travelers from areas where smallpox was endemic, while during this same period [1963-1978] at least 80 cases and three deaths resulted from three separate escapes from two different accredited smallpox laboratories.
The first recognized laboratory escape, in March 1972, occurred with the infection of a laboratory assistant at the London School of Hygiene and Tropical Medicine. She had observed the harvesting of live smallpox virus from eggs used as a growing medium; the process was performed on an uncontained lab table, as was then routine. Hospitalized, but before she was placed in isolation, she infected two visitors to a patient in an adjacent bed, both of whom died. They in turn infected a nurse, who survived, as did the laboratory assistant.
In August of 1978, a medical photographer at Birmingham Medical School developed smallpox and died. She infected her mother, who survived. Her workplace was immediately above the smallpox laboratory at Birmingham Medical School. Faulty ventilation and shortcomings in technique were ultimately implicated.
Investigators then re-examined a 1966 smallpox outbreak, which was strikingly similar. The initial 1966 infection was also a medical photographer who worked at the same Birmingham Medical School facility. The earlier outbreak was caused by a low-virulence strain of smallpox (variola minor), and it caused at least 72 subsequent cases. There were no deaths. Laboratory logs revealed variola minor [low virulence strain] had been manipulated in the smallpox laboratory at a time appropriate to cause the infection in the photographer working a floor above.”…
2007, Foot and Mouth disease escaped from high security UK lab at Pirbright:
[“At FMD laboratories near Pirbright...a commercial vaccine producer and a government-funded research institute share a facility.”]
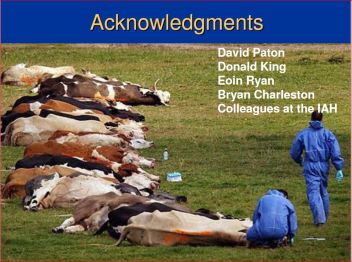 [Image: “The 2007 UK FMD outbreak, field investigation perspective“]
[Image: “The 2007 UK FMD outbreak, field investigation perspective“]
“In 2007, FMD appeared again in Britain, four kilometers [2.5. miles] from a biosafety level 4 laboratory—a designation indicating the highest level of lab security—located at Pirbright. The strain had caused a 1967 outbreak in the United Kingdom but was not then circulating in animals anywhere. It was, however, used in vaccine manufacture at the Pirbright facility. Investigations concluded that construction vehicles had carried mud contaminated with FMD from a defective wastewater line at Pirbright to the first farm. That outbreak identified 278 infected animals and required 1,578 animals to be culled. It disrupted UK agricultural production and exports and cost an estimated 200 million pounds [$284 million US].”…
[Added; Sep 7, 2007 (CIDRAP News) – “Britain’s recent outbreaks of foot-and-mouth disease (FMD) were likely caused by faulty wastewater drains at a laboratory facility, which contaminated soil that was then spread by trucks to a nearby cattle farm, British authorities announced today….DEFRA officials had previously linked the outbreaks to a leak from FMD laboratories near Pirbright where a commercial vaccine producer and a government-funded research institute share a facility....Though officials said faulty drain pipes were probably to blame for the FMD virus leak, investigators also found other problems at the Pirbright facilities, including several biosecurity breaches, such as inadequately monitored worker and vehicle movement and incomplete recordkeeping.…Construction trucks at the Pirbright site…were not washed or disinfected before leaving the area.”]
These narratives of escaped pathogens have common themes. There are unrecognized technical flaws in standard biocontainment, as demonstrated in the UK smallpox and FMD cases....Poor training of personnel and slack oversight of laboratory procedures negate policy efforts by national and international bodies to achieve biosecurity."…
……………………….
Full article:
3/31/2014, “Threatened pandemics and laboratory escapes: Self-fulfilling prophecies,” Martin Furmanski, Bulletin of the Atomic Scientists
“The public health danger from the escape, from laboratories, of viruses capable of causing pandemics has become the subject of considerable, well-merited discussion, spurred by “gain of function” experiments. The ostensible goal of these experiments— in which researchers manipulate already-dangerous pathogens to create or increase communicability among humans—is to develop tools to monitor the natural emergence of pandemic strains. Opponents, however, warn that the risk of laboratory escape of these high-consequence pathogens far outweighs any potential advance. These arguments appear in a variety of recent research papers, including Rethinking Biosafety in Research on Potential Pandemic Pathogens; The Human Fatality and Economic Burden of a Man-made Influenza Pandemic: A Risk Assessment; Containing the Accidental Laboratory Escape of Potential Pandemic Influenza Viruses; and Response to Letter by the European Society for Virology on “Gain-of-Function” Influenza Research.
The risk of a manmade pandemic sparked by a laboratory escape is not hypothetical: One occurred in 1977, and it occurred because of concern that a natural pandemic was imminent. Many other laboratory escapes of high-consequence pathogens have occurred, resulting in transmission beyond laboratory personnel. Ironically, these laboratories were working with pathogens to prevent the very outbreaks they ultimately caused. For that reason, the tragic consequences have been called “self-fulfilling prophecies.”
Modern genetic analysis allows pathogens to be precisely identified, and because all circulating pathogens show genetic changes over time, the year that a particular example of a pathogen emerged can generally be determined, given a sufficient database of samples. If a pathogen appears in nature after not circulating for years or decades, it may be assumed to have escaped from a laboratory where it had been stored inert for many years, accumulating no genetic changes; that is, its natural evolution had been frozen.
The swine flu scare of 1976 and the H1N1 human influenza pandemic of 1977.
Human H1N1 influenza virus appeared with the 1918 global pandemic, and persisted, slowly accumulating small genetic changes, until 1957, when it appeared to go extinct after the H2N2 pandemic virus appeared.
In 1976, H1N1 swine influenza virus struck Fort Dix [New Jersey, US], causing 13 hospitalizations and one death. The specter of a reprise of the deadly 1918 pandemic triggered an unprecedented effort to immunize all Americans. No swine H1N1 pandemic materialized, however, and complications of immunization truncated the program after 48 million immunizations, which eventually caused 25 deaths.
Human H1N1 virus reappeared in 1977, in the Soviet Union and [first observed in] China. Virologists, using serologic and early genetic tests soon began to suggest the cause of the reappearance was a laboratory escape of a 1949-1950 virus, and as genomic techniques advanced, it became clear that this was true. By 2010, researchers published it as fact: “The most famous case of a released laboratory strain is the re-emergent H1N1 influenza-A virus which was first observed in China in May of 1977 and in Russia shortly thereafter.” The virus may have escaped from a lab attempting to prepare an attenuated H1N1 vaccine in response to the [1976] US swine flu pandemic alert.
The 1977 pandemic spread rapidly worldwide but was limited to those under 20 years of age: Older persons were immune from exposures before 1957.
Its attack rate was high (20 to 70 percent) in schools and military camps, but mercifully it caused mild disease, and fatalities were few. It continued to circulate until 2009, when the pH1N1 virus replaced it.
There has been virtually no public awareness of the 1977 H1N1 pandemic and its laboratory origins, despite the clear analogy to current [2014] concern about a potential H5N1 or H7N9 avian influenza pandemic and “gain of function” experiments. The consequences of escape of a highly lethal avian virus with enhanced transmissibility would almost certainly be much graver than the 1977 escape of a “seasonal,” possibly attenuated strain to a population with substantial existing immunity.
Smallpox releases in Great Britain.
Eradication of natural smallpox transmission made the prospect of reintroduction of the virus intolerable. This risk was clearly demonstrated in the United Kingdom, where from 1963-1978 only four cases of smallpox (with no deaths) occurred that were imported by travelers from areas where smallpox was endemic, while during this same period at least 80 cases and three deaths resulted from three separate escapes from two different accredited smallpox laboratories.
The first recognized laboratory escape, in March 1972, occurred with the infection of a laboratory assistant at the London School of Hygiene and Tropical Medicine. She had observed the harvesting of live smallpox virus from eggs used as a growing medium; the process was performed on an uncontained lab table, as was then routine. Hospitalized, but before she was placed in isolation, she infected two visitors to a patient in an adjacent bed, both of whom died. They in turn infected a nurse, who survived, as did the laboratory assistant.
In August of 1978, a medical photographer at Birmingham Medical School developed smallpox and died. She infected her mother, who survived. Her workplace was immediately above the smallpox laboratory at Birmingham Medical School. Faulty ventilation and shortcomings in technique were ultimately implicated.
Investigators then re-examined a 1966 smallpox outbreak, which was strikingly similar. The initial 1966 infection was also a medical photographer who worked at the same Birmingham Medical School facility. The earlier outbreak was caused by a low-virulence strain of smallpox (variola minor), and it caused at least 72 subsequent cases. There were no deaths. Laboratory logs revealed variola minor had been manipulated in the smallpox laboratory at a time appropriate to cause the infection in the photographer working a floor above.
Venezuelan equine encephalitis in 1995.
Venezuelan equine encephalitis (VEE) is a viral disease transmitted by mosquitoes. It intermittently erupts in regional or continental-scale outbreaks that involve equines (horses, donkeys, and mules) in the Western Hemisphere. There are often concurrent zoonotic epidemics among humans. VEE in humans causes a severe febrile illness; it can occasionally be fatal or may leave permanent neurological disability (epilepsy, paralysis, or mental retardation) in 4 to 14 percent of clinical cases, particularly those involving children.
There were significant outbreaks of VEE every few years from the 1930s to the 1970s. Modern analysis revealed most outbreaks were genetic matches to the original 1938 VEE isolation used in inactivated veterinary vaccines. It was clear that many batches of the veterinary VEE vaccines had not been completely inactivated, so residual infective virus remained.
From 1938 to 1972, the VEE vaccine caused most of the very outbreaks that it was called upon to prevent, a clear self-fulfilling prophecy.
In 1995 a major VEE animal and human outbreak struck Venezuela and Colombia. There were at least 10,000 human VEE cases with 11 deaths in Venezuela and an estimated 75,000 human cases in Colombia, with 3,000 neurological complications and 300 deaths. VEE virus was isolated from 10 stillborn or miscarried human fetuses.
Genomic analysis identified the 1995 virus as identical to a 1963 isolate, with no indication it had been circulating for 28 years. It was another case of frozen evolution, but unlike the vaccine-related VEE outbreaks, the 1963 virus had never been used in a vaccine. Suspicion fell on an inadvertent release from a virology lab, either by an unrecognized infection of a lab worker or visitor, or escape of an infected laboratory animal or mosquito. The major scientific group working on VEE published a paper in 2001 stating the 1995 outbreak most likely was a laboratory escape, with considerable circumstantial evidence: The outbreak strain was isolated from an incompletely inactivated antigen preparation used on the open bench in the VEE laboratory located at the outbreak epicenter. But clear proof was lacking, and the group subsequently said it was reconsidering this conclusion.
SARS outbreaks after the SARS epidemic. The 2003 Severe Acute Respiratory Syndrome outbreak spread to 29 countries, causing more than 8,000 infections and at least 774 deaths. Because 21 percent of cases involved hospital workers, it had the potential to shut down health care services wherever it struck. It is particularly dangerous to handle in the laboratory because there is no vaccine, and it can be transmitted via aerosols.
Moreover, about five percent of SARS patients are “super-spreaders” who infect eight or more secondary cases. For instance, one patient spread SARS directly to 33 others (reflecting an infection rate of 45 percent) during a hospitalization, ultimately leading to the infection of 77 people, including three secondary super-spreaders. A super-spreader could turn even a single laboratory infection into a potential pandemic.
SARS has not re-emerged naturally, but there have been six escapes from virology labs: one each in Singapore and Taiwan, and four separate escapes at the same laboratory in Beijing.
The first was in Singapore in August 2003, in a virology graduate student at the National University of Singapore. He had not worked directly with SARS, but it was present in the laboratory where he worked. He recovered and produced no secondary cases. The World Health Organization formed an expert committee to revise SARS biosafety guidelines.
The second escape was in Taiwan in December 2003, when a SARS research scientist fell ill on a return flight after attending a medical meeting in Singapore. His 74 contacts in Singapore were quarantined, but again, fortunately, none developed SARS. Investigation revealed the scientist had handled leaking biohazard waste without gloves, a mask, or a gown. Ironically, the WHO expert committee called for augmented biosafety in SARS laboratories the day after this case was reported.
In April 2004, China reported a case of SARS in a nurse who had cared for a researcher at the Chinese National Institute of Virology (NIV). While ill, the researcher had traveled twice by train from Beijing to Anhui province, where she was nursed by her mother, a physician, who fell ill and died. The nurse in turn infected five third-generation cases, causing no deaths.
Subsequent investigation uncovered three unrelated laboratory infections in different researchers at the NIV. At least of two primary patients had never worked with live SARS virus. Many shortcomings in biosecurity were found at the NIV, and the specific cause of the outbreak was traced to an inadequately inactivated preparation of SARS virus that was used in general (that is, not biosecure) laboratory areas, including one where the primary cases worked. It had not been tested to confirm its safety after inactivation, as it should have been.
Foot and mouth disease in the UK in 2007. Foot and Mouth Disease (FMD) infects cloven-hoofed animals such as pigs, sheep, and cattle. It has been eradicated in North America and most of Europe. It is highly transmissible, capable of spreading through direct contact on the boots of farm workers and by natural aerosol that can spread up to 250 kilometers. Outbreaks in FMD-free areas cause economic disaster because meat exports cease and animals are massively culled. A 2001 UK outbreak resulted in 10 million animals killed and $16 billion in economic losses.
In 2007, FMD appeared again in Britain, four kilometers from a biosafety level 4 laboratory—a designation indicating the highest level of lab security—located at Pirbright. The strain had caused a 1967 outbreak in the United Kingdom but was not then circulating in animals anywhere. It was, however, used in vaccine manufacture at the Pirbright facility. Investigations concluded that construction vehicles had carried mud contaminated with FMD from a defective wastewater line at Pirbright to the first farm. That outbreak identified 278 infected animals and required 1,578 animals to be culled. It disrupted UK agricultural production and exports and cost an estimated 200 million pounds [$284 million US].
Federal law bans FMD virus from the continental United States, and it is held only at the US Department of Agriculture Plum Island facility off Long Island. Currently, however, its replacement, the National Bio and Agro-Defense Facility, is under construction in Manhattan, Kansas, under the aegis of the Department of Homeland Security. Moving FMD research to the agricultural heartland of the United States was opposed by many groups, including the Government Accountability Office, but Homeland Security decided on the Kansas location. In upgrading facilities to counter the threat of agro-bioterrorism, the department is increasing the risk to US agriculture of unintentional release.
Dangerous themes. These narratives of escaped pathogens have common themes. There are unrecognized technical flaws in standard biocontainment, as demonstrated in the UK smallpox and FMD cases. Inadequately inactivated preparations of dangerous pathogens are handled in laboratory areas with reduced biosecurity levels, as demonstrated in the SARS and VEE escapes. The first infection, or index case, happens in a person not working directly with the pathogen that infects him or her, as in the smallpox and SARS escapes. Poor training of personnel and slack oversight of laboratory procedures negate policy efforts by national and international bodies to achieve biosecurity, as shown in the SARS and smallpox escapes.
It is hardly reassuring that, despite stepwise technical improvements in containment facilities and increased policy demands for rigorous biosecurity procedures in the handling of dangerous pathogens, potentially high consequence breaches of biocontainment occur nearly daily: In 2010, 244 unintended releases of bioweapon candidate “select agents” were reported.
Looking at the problem pragmatically, the question is not if such escapes will result in a major civilian outbreak, but rather what the pathogen will be and how such an escape may be contained, if indeed it can be contained at all.
Experiments that augment virulence and transmissibility of dangerous pathogens have been funded and performed, notably with the H5N1 avian influenza virus. The advisability of performing such experiments at all—particularly in laboratories placed at universities in heavily populated urban areas, where potentially exposed laboratory personnel are in daily contact with a multitude of susceptible and unaware citizens—is clearly in question.
If such manipulations should be allowed at all, it would seem prudent to conduct them in isolated laboratories where personnel are sequestered from the general public and must undergo a period of exit quarantine before re-entering civilian life. The historical record tells us it is not a matter of if but when ignoring such measures will cost health and even lives. Perhaps many lives.”
…………………………………
“Editor’s note: This essay summarizes a more detailed review of the historical record with appropriate scientific references….The author thanks Lynn Klotz and Ed Sylvester for help with condensing the longer report for this article.” [“11 August 2014, doi: 10.3389/fpubh. 2014.00116, “The consequences of a lab escape of a potential pandemic pathogen,” Lynn C. Klotz1* and Edward J. Sylvester21, The Center for Arms Control and Non-Proliferation, Washington, DC, USA2, Science and Medical Journalism, Walter Cronkite School of Journalism and Mass Communication, Arizona State University, Phoenix, AZ, USA* Correspondence: lynnklotz@live.comEdited by:Kathleen Vogel, Cornell University, USA, Reviewed by: Kathleen Vogel, Cornell University, USA, Simon Wain-Hobson, Institut Pasteur, France.”
……………………………….
Added: Excerpt from “The consequences of a lab escape of a potential pandemic pathogen,” August 2014
“A 2013 Centers for Disease Control report is a significant source of recent data on LAIs [Lab-acquired infection] (11). The report documents four undetected or unreported LAIs in registered US Select Agent, high-containment BSL-3 labs between 2004 and 2010. An undetected or unreported LAI implies an escape when the infected person leaves the lab….
[page 2:] “The risk of a man-made pandemic from a lab escape is not hypothetical. Lab escapes of high-consequence pathogens resulting in transmission beyond lab personnel have occurred (20,21). The historical record reveals lab-originated outbreaks and deaths due to the causative agents of the 1977 pandemic flu,
smallpox escapes in Great Britain,
Venezuelan equine encephalitis in1995,
SARS outbreaks after the SARS epidemic, and
foot and mouth disease in the UK in 2007.
Ironically, these labs were working with pathogens to prevent the very outbreaks that they ultimately caused.”…

No comments:
Post a Comment